Vitamin A Deficiency: Comprehensive Guide to Symptoms, Risks, and Global Solutions
Vitamin A is a cornerstone of human health, playing a pivotal role in vision, immune function, cellular growth, and reproduction. Despite its critical importance, Vitamin A deficiency (VAD) remains a leading cause of preventable blindness, immune dysfunction, and child mortality worldwide. This in-depth article explores the symptoms of Vitamin A deficiency, the life-threatening risks of xerophthalmia, the populations most vulnerable to VAD, and actionable strategies to combat this global health crisis.
What is Vitamin A and Why Does It Matter?
Vitamin A is a fat-soluble nutrient existing in two primary forms:
Preformed Vitamin A (Retinol): Found in animal products like liver, eggs, and dairy.
Provitamin A Carotenoids (Beta-Carotene): Plant-based pigments in carrots, sweet potatoes, and leafy greens that the body converts into active Vitamin A.
This nutrient is essential for:
Vision: It forms rhodopsin, a protein in the retina that enables low-light and color vision.
Immune Health: Maintains mucosal barriers (eyes, lungs, gut) and supports white blood cell production.
Cell Growth: Regulates gene expression and cellular differentiation, vital for skin, organs, and fetal development.
Without adequate Vitamin A, the body becomes a ticking time bomb for systemic failure. Let’s dive deeper.
Symptoms of Vitamin A Deficiency: From Mild to Severe
Vitamin A deficiency progresses silently but destructively. Here’s a detailed breakdown of its symptoms and health consequences:
1. Early Warning Signs
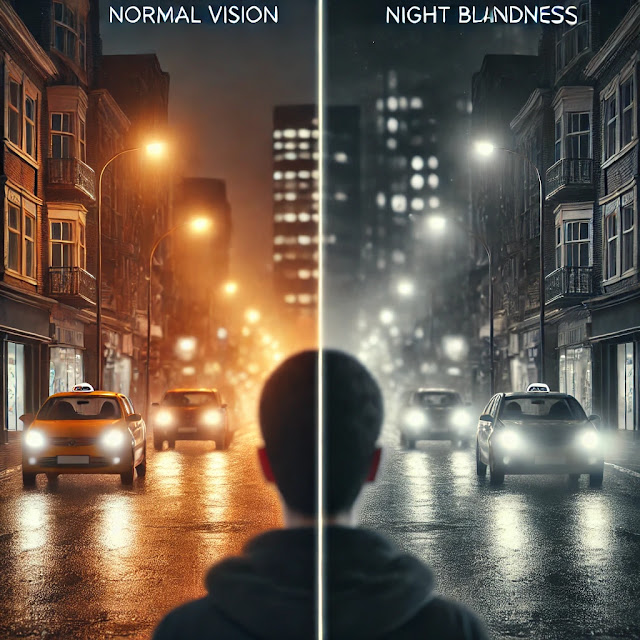
Night Blindness (Nyctalopia):
The earliest symptom, caused by impaired rhodopsin production.
Individuals struggle to see in dim light, increasing accident risks.
Dry Skin and Hyperkeratosis:
Rough, scaly skin (especially on elbows and knees) due to keratin buildup.
Dry, brittle hair and nails.
Frequent Infections:
Recurrent respiratory illnesses, diarrhea, and urinary tract infections due to weakened mucosal immunity.
2. Moderate to Severe Symptoms
Xerophthalmia: The hallmark of advanced VAD (explained in detail below).
Growth Retardation in Children:
Stunted bone development, delayed puberty, and reduced muscle mass.
Reproductive Issues:
In pregnant women, VAD raises risks of maternal mortality, preterm birth, and congenital disabilities.
Anemia:
Vitamin A aids iron metabolism; deficiency exacerbates anemia, causing fatigue and weakness.
3. Life-Threatening Complications
Corneal Ulceration and Blindness:
Untreated xerophthalmia leads to irreversible vision loss within 48 hours.
Severe Immune Suppression:
Fatal outcomes from measles, malaria, or diarrheal diseases due to collapsed immunity.
Increased Child Mortality:
VAD contributes to 2% of all deaths in children under 5 globally (WHO).
Xerophthalmia: The Eye Crisis in Vitamin A Deficiency
Xerophthalmia, derived from Greek (“dry eyes”), is the most dire consequence of Vitamin A deficiency. It progresses through irreversible stages:
Stages of Xerophthalmia
Night Blindness: Reversible with Vitamin A supplementation.
Conjunctival Xerosis:
Dry, thickened conjunctiva (the eye’s outer membrane).
Bitot’s Spots:
Foamy, white patches on the conjunctiva, signaling severe deficiency.
Corneal Xerosis:
Drying and clouding of the cornea.
Keratomalacia:
Corneal melting, ulceration, and perforation, leading to permanent blindness.
Why Xerophthalmia Demands Urgent Attention
Rapid Progression: Corneal damage can cause blindness in days.
High Mortality Link: 50–70% of children who go blind from xerophthalmia die within a year due to concurrent infections.
Geographic Hotspots: Over 140 million children in Africa and Southeast Asia have subclinical VAD, putting them at risk.
Who is Most at Risk for Vitamin A Deficiency?
While VAD affects all ages, these groups face disproportionate risks:
1. Children Under Five
Why: Rapid growth + high infection rates deplete Vitamin A stores.
Stats:
190 million preschool-aged children are Vitamin A-deficient (UNICEF).
South Asia and Sub-Saharan Africa account for 90% of affected children.
2. Pregnant and Lactating Women
Why: Increased nutrient demands for fetal development and breastfeeding.
Risks:
Night blindness affects 9.8% of pregnant women in low-income countries.
VAD raises risks of maternal hemorrhage and infant mortality.
3. Populations in Low-Income Countries
Dietary Limitations:
Reliance on grains (rice, wheat) lacking beta-carotene.
Limited access to animal-sourced foods (meat, dairy).
Economic Barriers:
Poverty restricts access to fortified foods or supplements.
4. Individuals with Health Conditions
Malabsorption Disorders: Celiac disease, Crohn’s, or cystic fibrosis impair fat-soluble vitamin uptake.
Chronic Infections: Measles and HIV accelerate Vitamin A depletion.
Global Solutions to Combat Vitamin A Deficiency
Eradicating VAD requires a multi-pronged approach:
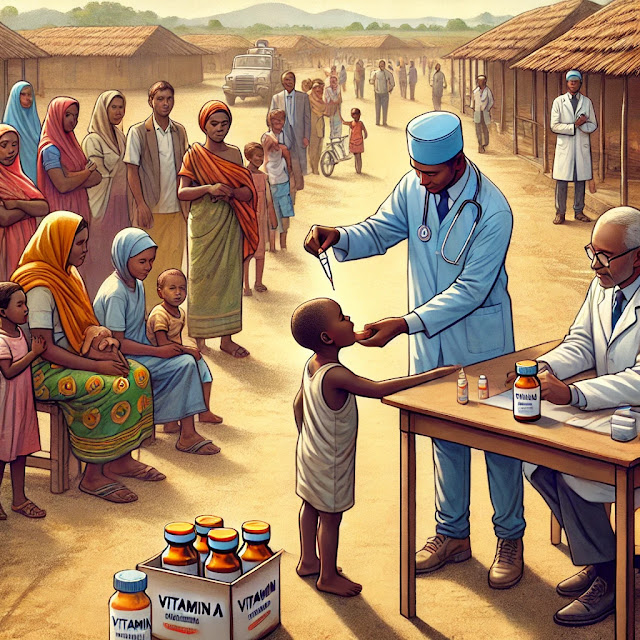
1. High-Dose Vitamin A Supplementation (VAS)
How It Works: Biannual capsules providing 100,000–200,000 IU of Vitamin A.
Impact: Reduces child mortality by 12–24% (Cochrane Review).
Challenges: Reaching remote communities and sustaining funding.
2. Food Fortification
Successful Models:
Vitamin A-fortified cooking oil in Indonesia reduced deficiency rates by 50%.
Golden Rice: Genetically modified rice with beta-carotene (approved in the Philippines).
3. Dietary Diversification
Home Gardens: Promoting crops like orange-fleshed sweet potatoes, carrots, and spinach.
Animal-Source Foods: Encouraging poultry farming and egg consumption in rural areas.
4. Public Health Education
Breastfeeding Advocacy: Colostrum is rich in Vitamin A.
Cooking Workshops: Teaching methods to preserve beta-carotene (e.g., steaming vs. boiling).
5. Policy and Funding
UNICEF and WHO Programs: Distributing 500 million Vitamin A capsules annually.
Government Partnerships: Subsidizing fortified foods in schools.
Vitamin A-Rich Foods to Include in Your Diet
Preventing VAD starts on your plate. Top sources include:
Animal Sources: Beef liver, fish liver oil, eggs, and dairy.
Plant Sources: Sweet potatoes, carrots, kale, spinach, and mangoes.
Fortified Foods: Cereals, margarine, and milk in fortified regions.
FAQs About Vitamin A Deficiency
Can you overdose on Vitamin A?
Yes. Excess preformed Vitamin A (retinol) causes toxicity, but beta-carotene is safe.
How is VAD diagnosed?
Blood tests (serum retinol levels) and clinical signs like Bitot’s spots.
Are supplements safe during pregnancy?
Yes, but high doses should be medically supervised to avoid birth defects.
Conclusion: A Vision for a Healthier Future
Vitamin A deficiency is a solvable global crisis. Xerophthalmia and immune collapse are preventable with cost-effective strategies like supplementation, fortification, and education. By prioritizing nutrition in policy and empowering communities to grow Vitamin A-rich foods, we can save millions of lives—and preserve the gift of sight.